- #1
sameeralord
- 662
- 3
Hello everyone,
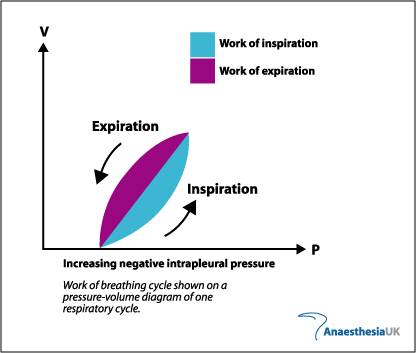
Now at higher lung volumes intrapleural pressure must be positive. But according to the graph as inspiration increases intrapleural pressure is becoming more negative?
Please help! Thanks
Now at higher lung volumes intrapleural pressure must be positive. But according to the graph as inspiration increases intrapleural pressure is becoming more negative?
Please help! Thanks