sameeralord said:
Hello everyone,
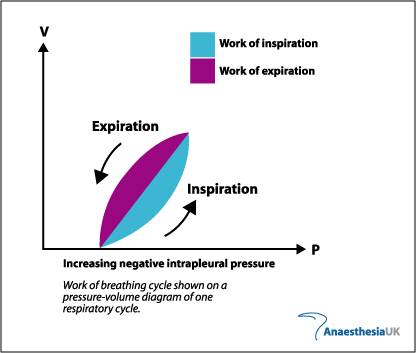
Now at higher lung volumes intrapleural pressure must be positive. But according to the graph as inspiration increases intrapleural pressure is becoming more negative?
Please help! Thanks

No intrapleural pressure (Pi) is negative, as in subatmospheric (atmospheric defined as 0). It's normally around -5, during inhalation it goes to around -8.
The pressure in alveoli (PA) is equilibriated with Patm at resting position and goes to -1 to -2 during inhalation.
As the diaphragm pulls down it expands the thoracic cavity making the Pi more subatmospheric. Since the parietal pleura (which lines the thoracic wall) is adhered to the visceral pleura the distending forces (Pi becoming more subatm) overcome the collapsing forces (the surface tension on the surface of the alveoli, which is also why you have pulmonary surfactant there) and lungs expand.
The transmural pressure, Pt, which is the difference between PA and Pi, so during resting position;
0-(-5)=5, during inhalation;
-1-(-8)=7.
Expiration is normally a passive event and relies on the recoil of the thoracic cavity and collapsing pressure of the alveoli (when the radius of alveoli get large, the wall tension can overcome the relief provided by pulmonary surfactant and aid in lung recoil).
During forced expiration (mostly through the work of your abdominal muscles and inner intercostals muscles) you can actually create very high positive Pi and PA, around 25 and 30 respectively.
In parts the Pi can actually equal the PA which means the Pt (when 0 or negative) favors collapse of that portion of the tracheobronchial tree, but cartilage rings hold it open.
So for your graph, you see that Pi is actually becoming more negative (more subatmospheric) when we inhale and less subatmospheric (even positive at times) when exhale.
Remember what's important though the pressure gradients and transmural pressure across the alveoli (which distends/collapse the alveoli) wall that matter for breathing.
As a side note; I swear Sameeralord everytime you ask a question, you're like my subconscious reminding me of stuff I need to review for boards, lol