- #1
coolia
- 19
- 0
I posted this question in the physics forum with no luck, the concept has to do with physics but it's applications is within the body. It is found in the lung and also in venous return curves, when central venous pressure drops below 0. Basically, I am asking how the concept of zone 2 in the lung works, where the effective driving pressure is given by the difference between arterial pressure and alveolar pressure and not venous pressure. In fact, they say venous pressure has no effect on flow. I am confused on how this works so if anyone could give me an explanation that would be helpful. Below is my original post that gives my thoughts about and an image.
-------------------------------------------------------------------------------------
My question is in regards to a starling resistor. A starling resistor is where a flexible tube passes through a box that can have it's pressure changed. If fluid passes through the tube then flow through the box will be determined by the pressure differences from the two sides of the box provided the pressure on both sides of the tube outside the box are greater than the pressure in the box.
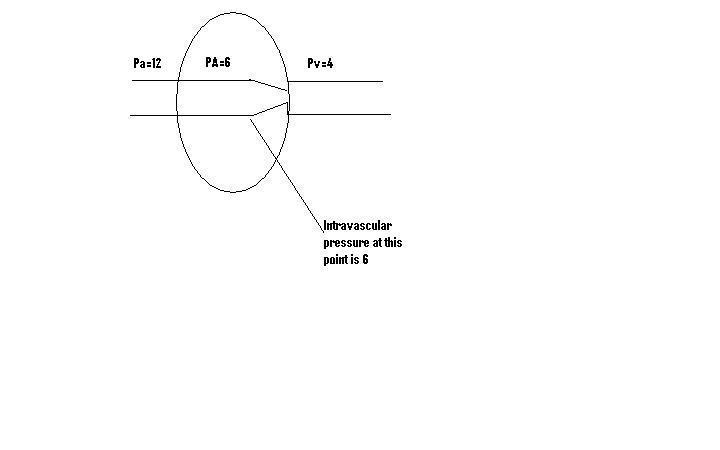
If pressure in the box becomes greater than the downstream pressure of the tube coming out of the box then flow will be determined by the difference between the upstream pressure and the pressure in the box. The tube will collapse at a point where the pressure in the tube becomes less than the pressure in the box (this is a pressure of 6 in the diagram below). The downstream pressure will not affect flow through the tube. I attached an image that goes along with the above explanation. Pa(arterial)=upstream pressure, Pv(venous)=downstream pressure and PA(alveolar)=pressure in the box. The above occurs physiologically in bodies most popularly in the capillaries of the lungs (zone 2). My question is how is the upstream pressure - pressure in the box the driving pressure (as they say it is) when the pressure driving flow through a tube should be difference between the pressure at the two ends of the tube? Does the collapse occur gradually, in other words is end closest to the box a smaller opening than more upstream. Also, I'm assuming the resistance increases in the tube because of the collapse and this would be the cause of the decreased flow and not a change in pressure because the downstream and upstream pressure are the same. There would also be a greater drop in pressure from the collapsed ends than from the open ends, due to the collapsed ends having a greater resistance. Is this correct?
Thank you.
-------------------------------------------------------------------------------------
My question is in regards to a starling resistor. A starling resistor is where a flexible tube passes through a box that can have it's pressure changed. If fluid passes through the tube then flow through the box will be determined by the pressure differences from the two sides of the box provided the pressure on both sides of the tube outside the box are greater than the pressure in the box.
If pressure in the box becomes greater than the downstream pressure of the tube coming out of the box then flow will be determined by the difference between the upstream pressure and the pressure in the box. The tube will collapse at a point where the pressure in the tube becomes less than the pressure in the box (this is a pressure of 6 in the diagram below). The downstream pressure will not affect flow through the tube. I attached an image that goes along with the above explanation. Pa(arterial)=upstream pressure, Pv(venous)=downstream pressure and PA(alveolar)=pressure in the box. The above occurs physiologically in bodies most popularly in the capillaries of the lungs (zone 2). My question is how is the upstream pressure - pressure in the box the driving pressure (as they say it is) when the pressure driving flow through a tube should be difference between the pressure at the two ends of the tube? Does the collapse occur gradually, in other words is end closest to the box a smaller opening than more upstream. Also, I'm assuming the resistance increases in the tube because of the collapse and this would be the cause of the decreased flow and not a change in pressure because the downstream and upstream pressure are the same. There would also be a greater drop in pressure from the collapsed ends than from the open ends, due to the collapsed ends having a greater resistance. Is this correct?
Thank you.
