- #1
jaumzaum
- 434
- 33
Hello guys, can anyone help me to understand why an increase in peripheral resistance causes an increase in the blood pressure?
If we assume the equation
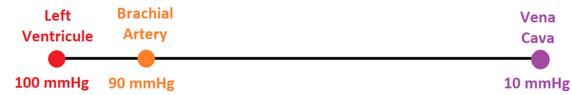
Delta P = R times Q
If we assume Q is constant, the greater the resistance the greater the the decrease in pressure, so the pressure should be lower not higher
The only explanation I would have for the blood pressure to increase would be the heart trying to increase the aortic pressure so that the cava vein pressure (usually less than 4 mmHg) remains positive, and so the increase in blood pressure would be an indirect effect created because the heart itself begins to pump stronger. Is that right?
If we assume the equation
Delta P = R times Q
If we assume Q is constant, the greater the resistance the greater the the decrease in pressure, so the pressure should be lower not higher
The only explanation I would have for the blood pressure to increase would be the heart trying to increase the aortic pressure so that the cava vein pressure (usually less than 4 mmHg) remains positive, and so the increase in blood pressure would be an indirect effect created because the heart itself begins to pump stronger. Is that right?